Soap Charting Method . there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. wondering how to write soap notes? Subjective, objective, assessment, and plan. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Getting the soap format right is essential for therapists. A soap note is standard across all types of chart. Here are soap note examples.
from studylib.net
Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. A soap note is standard across all types of chart. wondering how to write soap notes? Here are soap note examples. Subjective, objective, assessment, and plan. there are four basic components of a soap note: — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a.
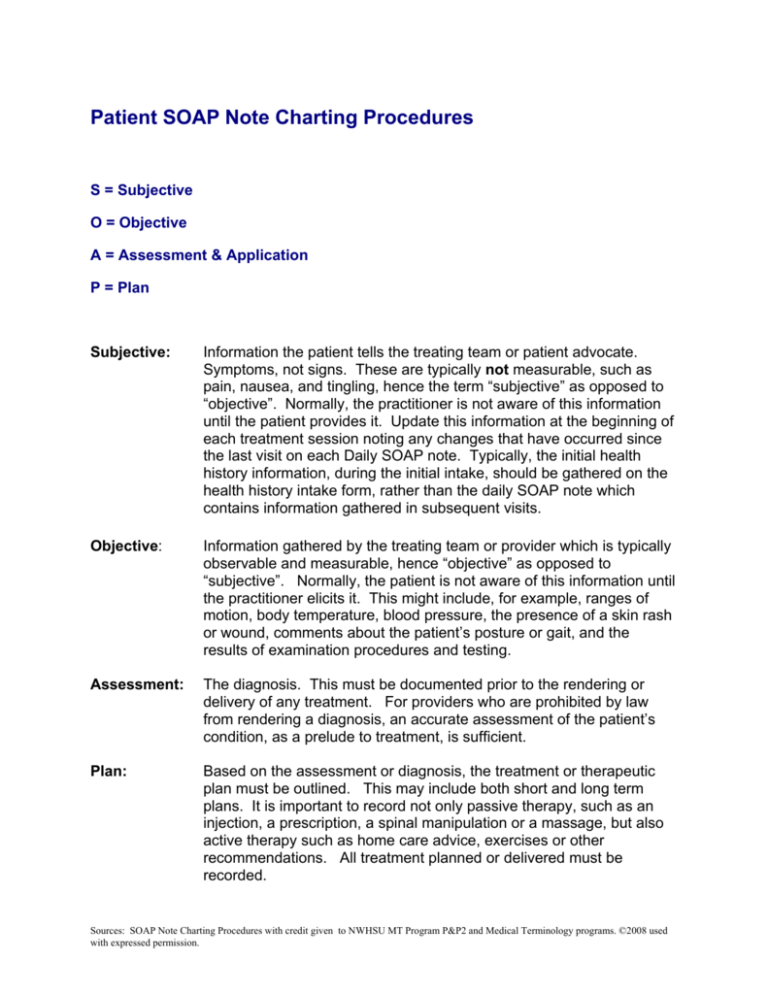
Patient SOAP Note Charting Procedures
Soap Charting Method Getting the soap format right is essential for therapists. wondering how to write soap notes? there are four basic components of a soap note: Subjective, objective, assessment, and plan. Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Getting the soap format right is essential for therapists.
From slideplayer.com
Chapter 13 Managing Medical Records ppt download Soap Charting Method Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. wondering how to write soap notes? there are four basic components of a soap note: Here are soap note examples. soap notes are a highly structured format for documenting the progress. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. wondering how to write soap notes? Getting the soap format right is essential for therapists. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Here are soap note. Soap Charting Method.
From quizzmediasophie.z13.web.core.windows.net
The E Entry In The Soaper Charting Method Means Soap Charting Method Getting the soap format right is essential for therapists. wondering how to write soap notes? Subjective, objective, assessment, and plan. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: — soap—or subjective, objective, assessment and plan—notes allow clinicians to document. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Getting the soap format right is essential for therapists. A soap note is standard across all types of chart. wondering how to write soap notes?. Soap Charting Method.
From lucadavies.z19.web.core.windows.net
The R Entry In The Soaper Charting Method Means Soap Charting Method Getting the soap format right is essential for therapists. there are four basic components of a soap note: soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Here are soap note examples. A soap note is standard across all types of chart. Subjective, objective, assessment,. Soap Charting Method.
From www.pinterest.com
SOAP vs SBAR Nursing school survival, Nursing school tips, Nursing Soap Charting Method Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. A soap note is standard across all types of chart. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: Here are soap note examples. — soap—or subjective,. Soap Charting Method.
From tucsonceu.com
Integrating Interview Skills & SOAP Charting into your Treatment Plan Soap Charting Method Getting the soap format right is essential for therapists. Subjective, objective, assessment, and plan. Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: soap notes are a highly structured format for documenting the progress of a. Soap Charting Method.
From www.powerdiary.com
Clinical Notes Resources and Templates for Practitioners Power Diary Soap Charting Method A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. there are four basic components of a soap note: soap notes are a highly. Soap Charting Method.
From dxoghuaue.blob.core.windows.net
Soap Define Method at Victoria Yin blog Soap Charting Method Here are soap note examples. Subjective, objective, assessment, and plan. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. A soap note is standard across all types of chart.. Soap Charting Method.
From www.etsy.com
SOAP Notes Etsy Soap Charting Method soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. wondering how to write soap notes? — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing. Soap Charting Method.
From www.slideserve.com
PPT Medical Records and Documentation PowerPoint Presentation, free Soap Charting Method Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. soap notes are a highly structured format for documenting the. Soap Charting Method.
From slideplayer.com
Chapter 13 Managing Medical Records ppt download Soap Charting Method A soap note is standard across all types of chart. Here are soap note examples. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Subjective, objective, assessment, and plan. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Getting the soap format right is. Soap Charting Method.
From www.slideserve.com
PPT Nursing Fundamentals Chapter 9 Recording & Reporting PowerPoint Soap Charting Method A soap note is standard across all types of chart. Getting the soap format right is essential for therapists. there are four basic components of a soap note: — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. wondering how to write soap notes? — the subjective, objective, assessment and. Soap Charting Method.
From www.advantismed.com
How to Master Nurse Charting & Avoid Mistakes Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. Getting the soap format right is essential for therapists. wondering how to write soap notes? A soap note is standard across all types of chart. soap notes are a highly structured format for documenting the progress of a patient during treatment. Soap Charting Method.
From www.slideserve.com
PPT SOAP Charting PowerPoint Presentation, free download ID2302720 Soap Charting Method Here are soap note examples. wondering how to write soap notes? A soap note is standard across all types of chart. Subjective, objective, assessment, and plan. — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in. Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method there are four basic components of a soap note: — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Getting the soap format right is essential for therapists. A. Soap Charting Method.
From www.powerdiary.com
Essential Guide to SOAP Notes SOAP Notes Example Soap Charting Method Here are soap note examples. there are four basic components of a soap note: A soap note is standard across all types of chart. — soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. Getting the soap format right is essential for therapists. — the subjective, objective, assessment and plan (soap). Soap Charting Method.
From hamiltonplastering.com
35 soap Charting Examples Hamiltonplastering Soap Charting Method — the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used. A soap note is standard across all types of chart. Here are soap note examples. soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Subjective, objective, assessment, and plan.. Soap Charting Method.